The Meditation-Longevity Connection: Your Brain’s Secret Weapon Through Every Hormonal Chapter
*A journey from ancient wisdom to modern neuroscience—and what the evidence actually shows about women, hormones, and the practice of presence
Before Meditation Was Medicalized: A Global History
Here’s what most wellness content won’t tell you: meditation isn’t some ancient Eastern secret that the West just discovered. Humans have been experimenting with focused attention, controlled breathing, and intentional stillness across virtually every culture for millennia—for reasons far more varied than stress reduction.
### The Greek Contemplative Tradition
Long before “mindfulness” became a Silicon Valley buzzword, ancient Greek philosophers were exploring states of focused awareness they called *theōría* (θεωρία)—contemplation.
For Plato, contemplation was the recollection of eternal truths, a withdrawal from sensory distraction to access higher knowledge. Aristotle considered *theōría* the highest human activity, intimately linked to *eudaimonia*—human flourishing.
The Orphic and Eleusinian mystery traditions involved ritualized experiences of silence, darkness, and symbolic transformation. While these weren’t meditation as we’d define it today, they represent a parallel understanding: that deliberate alterations of consciousness through controlled sensory experience could produce profound psychological and possibly physiological effects.
**Important distinction:** Equating Greek contemplation with modern meditation is anachronistic. These were philosophical and ritual technologies of meaning-making, not the standardized attention-training protocols studied in neuroscience labs today. But the conceptual bridge matters—humans have long intuited that training the mind changes the person.
### Eastern Origins: Where Technique Met System
The practices we now call meditation emerged most systematically in ancient India and China:
**India’s Vedic and Buddhist traditions** developed *dhyāna*—disciplined mental training involving breath regulation, focused attention, and progressive states of absorption. These weren’t wellness practices; they were technologies aimed at liberation from suffering, with detailed maps of consciousness and surprisingly specific “dosing” instructions.
**Daoist inner cultivation** in China explicitly linked breath control, attention, and longevity—viewing the body as a microcosm of natural forces that could be harmonized through practice. The connection between contemplative practice and lengthened lifespan isn’t a modern invention; it’s baked into these traditions’ foundational texts.
**Across the Islamic world**, Sufi contemplative practices involved *dhikr* (remembrance), rhythmic breathing, and focused attention—again, with the explicit goal of transformation, not just relaxation.
### Indigenous and African Traditions: The Missing Narratives
Here’s where the standard meditation-for-wellness story gets really incomplete.
Indigenous cultures worldwide developed contemplative and trance-inducing practices deeply embedded in community, ritual, and ecological connection:
- **African spiritual traditions** incorporated rhythmic drumming, dance, breathwork, and communal ceremony to induce altered states—practices that engaged the nervous system through embodied, relational experience rather than solitary stillness
- **Native American vision quests** combined fasting, isolation, and focused intention—creating conditions for profound psychological and physiological shifts
- **Australian Aboriginal dreamtime practices** involved specific attentional states for accessing ancestral knowledge and connection
These traditions understood something modern neuroscience is only now confirming: **the nervous system can be trained through culturally-specific practices, and the “best” method depends entirely on context, community, and what you’re training it for.**
The colonization of contemplative practice into “mindfulness-based interventions” has largely erased this diversity. What we study in labs represents a tiny, culturally-specific slice of human contemplative technology—predominantly drawn from Buddhist vipassanā and Zen traditions, filtered through secular Western clinical contexts.
**Why this matters for women’s longevity:** Different cultural approaches to contemplative practice emphasize different nervous system pathways. Some prioritize stillness and withdrawal (stereotypically “Eastern”). Others emphasize embodied, relational, rhythmic engagement (common in African and Indigenous traditions).
For women navigating midlife transitions—when embodiment becomes fraught, when isolation increases, when community and rhythm might matter as much as breath control—this diversity of approaches isn’t academic. It’s practical.
-----
## What Neuroscience Actually Studies (And What It Doesn’t)
When researchers study “meditation,” they’re not studying enlightenment or spiritual communion. They’re studying operationalized, standardized practices under controlled conditions.
**Critical point:** These are not interchangeable. Different practices engage different neural networks and may produce different biological effects. Lumping them together as “meditation” is like calling all exercise “movement” and expecting a yoga class to produce the same cardiovascular adaptations as interval training.
-----
## The Neuroscience: What’s Solid, What’s Suggestive, What’s Overhyped
Let’s separate the signal from the wellness-industrial noise.
Emotion Regulation: Strong Evidence ✓
This is where the data are most consistent.
Meditation reliably alters how the brain processes and regulates emotional experience:
- **Reduced amygdala reactivity** to emotional stimuli (particularly threatening or distressing content)
- **Increased functional connectivity** between the amygdala and prefrontal regulatory regions
- **Enhanced ability to downregulate negative emotion** without suppression
This represents genuine neuroplasticity—the brain learning to respond rather than react. For women navigating the emotional volatility of hormonal transitions, this matters enormously.
### Default Mode Network Changes: Robust and Replicated ✓
One of meditation’s most reproducible neural signatures involves the **Default Mode Network (DMN)**—the brain regions active during mind-wandering, self-referential thinking, and rumination.
Regular meditation practice is associated with:
- Decreased activity in medial prefrontal cortex and posterior cingulate cortex during meditation
- Reduced mind-wandering and ruminative thought patterns
- Greater ability to disengage from unhelpful mental narratives
This finding has held up across multiple labs, techniques, and populations. It’s as close to consensus as neuroscience gets.
**Why it matters for longevity:** Rumination and chronic worry are strongly associated with accelerated cellular aging, elevated inflammatory markers, and increased disease risk. A practice that demonstrably reduces rumination isn’t just making you feel better—it’s potentially reducing biological wear and tear.
Structural Brain Changes: Mixed Evidence (Correction Needed)
Earlier enthusiasm about meditation “growing your brain” needs significant temperament.
**What some studies show:**
- Modest increases in cortical thickness in attention and emotion-regulation regions
- Possible hippocampal volume preservation in long-term practitioners
**What systematic reviews and large analyses actually find:**
- Many well-designed studies show **no significant structural changes**
- When changes appear, effect sizes are small and heavily dependent on practice duration and intensity
- Publication bias likely inflates positive findings
**Honest assessment:** Structural brain changes from meditation are *possible*, not *guaranteed*, and not something you should expect from 10 minutes a day for a month. The functional changes (how your brain operates) are far more reliable than anatomical ones.
### Autonomic Nervous System & Vagal Tone: Correction Required
Here’s where popular narratives outpace the data.
**Common claim:** “Meditation increases vagal tone and heart rate variability (HRV), improving nervous system regulation.”
**What meta-analyses actually show:** Large-scale reviews of randomized controlled trials find **no significant effect** of meditation on resting-state HRV across populations.
Some individual studies show effects, but they’re inconsistent, context-dependent, and often confounded by other variables (sleep quality, exercise, stress reduction).
**More accurate framing:** Meditation reliably improves *subjective* stress regulation and emotional flexibility. It does not consistently alter autonomic nervous system biomarkers like HRV in predictable ways across diverse populations.
This doesn’t make meditation ineffective—it just means the mechanism isn’t primarily about vagal tone modulation as popularly claimed.
-----
## Where the Evidence Gets Really Interesting: Inflammation, Stress Biology, and Cellular Aging
Cortisol and Inflammatory Markers: Strong Evidence ✓
This is where meditation’s longevity relevance becomes genuinely compelling.
Across multiple trials and meta-analyses, meditation-based interventions consistently show:
- **Reduced cortisol** (the primary stress hormone)
- **Decreased pro-inflammatory markers** (IL-6, C-reactive protein, TNF-α)
- **Increased anti-inflammatory signaling** (IL-10 in some contexts)
These effects are:
- Moderate in size (not miracle-level, but clinically meaningful)
- More robust in high-stress or clinical populations
- Consistent across MBSR-style interventions
**For women in midlife:** Chronic low-grade inflammation (“inflammaging”) and elevated cortisol are primary drivers of accelerated aging, cardiovascular disease, cognitive decline, and metabolic dysfunction. A practice that measurably reduces both—without pharmaceuticals—deserves serious attention.
Telomeres and Cellular Aging: Promising But Not Definitive
This is where the science gets fascinating—and where claims need careful handling.
**The often-cited finding:** A 2013 study by Dean Ornish and colleagues found that comprehensive lifestyle intervention was associated with increased telomerase activity (the enzyme that maintains telomere length) and telomere lengthening over five years.
**Critical caveat:** This wasn’t a “meditation study.” It was a comprehensive program including:
- Plant-based diet
- Moderate exercise
- Stress management (which included meditation)
- Social support groups
Meditation was one component among many. Attributing the results solely to meditation is scientifically dishonest.
**What the broader literature shows:**
- Some studies associate meditation with increased telomerase activity or slower telomere shortening
- Results are heterogeneous—highly variable by study design, population, and practice intensity
- The mechanism likely involves reduced chronic stress and inflammation rather than direct cellular effects
**Responsible claim:** Meditation may support cellular aging pathways *indirectly*, primarily through stress reduction and improved health behaviors. It is not a stand-alone longevity intervention, but a meaningful component of a systems-level approach to healthspan.
-----
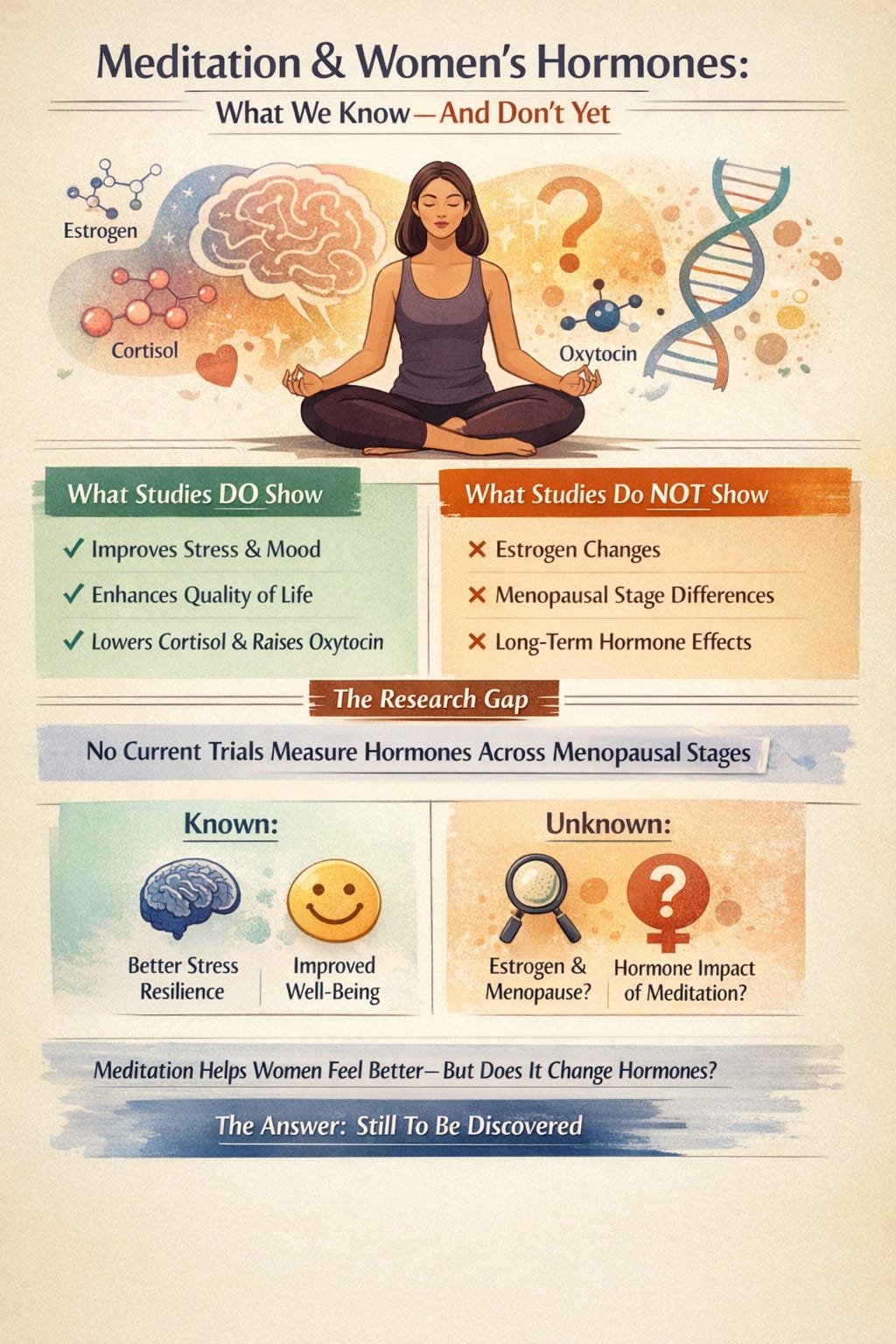
Meditation, Women’s Hormones & Life Stage: What We Know, What We Don’t
Here’s the section most wellness content either ignores or wildly overstates.
Cortisol: The Most Consistent Endocrine Signal ✓
Among hormonal outcomes, **cortisol reduction is the most reproducible finding**.
- A randomized controlled trial of Heartfulness meditation demonstrated significant reduction in serum cortisol after 30 days in adult women
- Mindfulness-based interventions consistently reduce perceived stress, anxiety, and depressive symptoms in perimenopausal and postmenopausal women
- While many studies infer cortisol reduction indirectly (via validated psychological measures), this aligns with broader research linking reduced psychological stress to lower HPA-axis activation
**Bottom line:** Meditation reliably reduces stress load in women, and cortisol modulation is the most evidence-supported hormonal pathway—particularly during midlife transitions.
Oxytocin: Emerging But Intriguing Evidence
Oxytocin—often called the “bonding hormone”—is rarely measured in behavioral intervention trials, making recent findings notable.
The same Heartfulness meditation study reported a **significant increase in serum oxytocin** after 30 days of practice in women, correlating with improvements in positive affect and emotional regulation.
**Careful interpretation:**
- This is practice-specific evidence (Heartfulness meditation uses heart-focused techniques), not a universal meditation effect
- Replication is needed
- But the data support the hypothesis that certain relational or heart-focused practices may engage oxytocinergic pathways
**Why this matters:** Oxytocin appears to buffer stress reactivity, support immune function, and influence inflammation and cellular repair processes. For women—whose social connection and caregiving roles are often sources of both stress and resilience—practices that increase oxytocin while reducing cortisol create a particularly favorable neurochemical profile.
### Estrogen: No Direct Modulation Demonstrated
Here the evidence is clear—and often wildly misrepresented elsewhere.
What we know:**
- **No clinical studies demonstrate that meditation directly alters estrogen or estradiol levels** in women at any life stage
- However, one well-designed RCT found that women with greater mood sensitivity to estradiol fluctuations experienced greater psychological benefit from MBSR
What this means:**
Meditation does not change estrogen levels. But it may buffer the brain’s response to hormonal variability—particularly during perimenopause, when estrogen swings create neurological whiplash.
**Key distinction:** Meditation is a **neuroregulatory intervention**, not endocrine replacement therapy. It changes how the brain *responds* to hormonal fluctuations, not the hormones themselves.
### Life Stage Matters (Even If Data Are Sparse)
Across trials and meta-analyses, **perimenopausal and postmenopausal women show the most consistent psychological benefit** from mindfulness-based interventions.
Documented improvements include:
- Mood stability
- Sleep quality
- Reduced distress from hot flashes (subjective experience, not frequency)
- Overall quality of life
These effects likely arise from **central nervous system regulation of stress and affect**, not peripheral hormone production.
The Research Gap Nobody Talks About
Despite dozens of studies on meditation and menopausal symptoms, **there are currently no registered clinical trials specifically designed to measure how meditation alters estrogen, cortisol, or other key hormones across different reproductive stages**.
What studies rigorously measure:
- Symptom severity (vasomotor distress, sleep, mood)
- Psychological well-being and quality of life
- Perceived stress and depression
What they largely don’t measure:
- Actual hormone levels pre- vs. post-intervention
- How menopausal stage modifies the response
- Long-term neuroendocrine changes stratified by life stage
**The one major trial examining mindfulness in menopausal women** (NCT06421909) focuses entirely on psychological and symptomatic outcomes—no hormone measurements included.
**Translation:** Meditation consistently helps women *feel and function* better during hormonal transitions. Whether it directly *changes hormone levels* in stage-specific ways remains scientifically open.
This isn’t a failure of meditation research—it reflects how young women-specific psychoneuroendocrinology still is.
The Longevity Case Across Life Stages: A Biologically Honest Model
In Your 30s and 40s (Pre-Perimenopause)
This is your **neuroplasticity sweet spot**. Regular practice now builds neural infrastructure—stress resilience circuits, emotional regulation capacity—that you’ll desperately want when hormones start their rollercoaster.
You’re essentially installing shock absorbers before the rough terrain begins.
The brain changes most readily documented in this age group:
- Enhanced prefrontal-amygdala connectivity
- Reduced default mode network hyperactivity
- Improved attention regulation
During Perimenopause (The Wild Years)
When your hypothalamus is trying to make sense of erratic estrogen signals, **meditation offers your brain an anchor**.
Studies show consistent practice can reduce hot flash *distress* and frequency—not by altering hormones directly, but by calming the nervous system’s overreaction to hormonal fluctuations.
You’re teaching your brain that not every estrogen dip is a five-alarm fire.
### Postmenopause (The Recalibration)
With estrogen’s neuroprotective effects diminished, your brain is more vulnerable to stress-accelerated aging.
This is when meditation’s **cortisol-lowering, inflammation-dampening effects** become particularly protective. You’re actively maintaining the brain resilience you’ll need for cognitive longevity.
Documented benefits in this population:
- Sustained mood stability
- Better sleep architecture
- Reduced inflammatory burden
- Maintained cognitive flexibility
## The Practice That Matters More Than the Style
Here’s the good news: you don’t need to achieve enlightenment or sit in perfect lotus position.
**What appears to matter most:**
**Consistency over intensity** → Daily 10-20 minutes beats sporadic hour-long sessions
**Breath-focused practices** → These directly engage your vagus nerve and parasympathetic nervous system (even if they don’t reliably increase HRV)
**Non-striving attitude** → The goal is presence, not performance. Midlife women especially don’t need another achievement to stress about.
**Cultural resonance** → The “best” practice is the one that feels authentic to your background, values, and nervous system needs. For some women, that’s silent seated meditation. For others, it’s rhythmic movement, communal practice, or embodied contemplation.
The Heartfulness study that showed hormonal changes used a specific protocol: 30 minutes daily of heart-focused meditation with relaxation techniques. But mindfulness-based stress reduction (MBSR), loving-kindness meditation, and even simple breath awareness all show benefits in women’s health studies.
**The best practice is the one you’ll actually do.**
## What Science Needs to Do Next (And Why It Matters)
The research gap isn’t trivial—**it’s an equity issue**.
We have extensive data on meditation’s effects in mixed-gender populations and in men. We have decades of longevity research that barely accounts for hormonal variability in female participants.
**What’s desperately needed:**
- Trials that stratify participants by menopausal status
- Longitudinal studies tracking neuroendocrine markers across hormonal transitions
- Research examining whether meditation’s effects differ based on reproductive timeline
- Investigation of optimal timing, frequency, and style for different life stages
- **Studies that honor cultural diversity in contemplative practices** rather than defaulting to secularized Buddhist-derived techniques
Until then, we’re working with suggestive evidence, biological plausibility, and consistent (if incomplete) data on symptom improvement.
That’s not nothing. But it’s not everything either.
## The Bottom Line: Ancient Wisdom, Modern Evidence, Your Second Act Brain
Across cultures and millennia, humans intuited something neuroscience is now confirming: **the brain can be trained, and that training has biological consequences**.
Greek philosophers called it contemplation. Indian practitioners called it dhyāna. Indigenous traditions embedded it in rhythm, community, and ceremony. Modern science calls it neuroplasticity.
Different language. Same nervous system.
**For women navigating midlife:**
Menopause isn’t decline—it’s biological reorganization. Your brain is literally rewiring itself for a post-reproductive life stage that, for the first time in human history, can span 40+ years.
The question isn’t whether you’ll go through this transition. It’s whether you’ll go through it with a nervous system trained for resilience—or one marinating in chronic stress.
**What meditation won’t do:**
- Replace hormone therapy
- Guarantee structural brain changes
- Directly alter your estrogen levels
- Stop you from aging
**What it can do—reliably:**
- Reduce cortisol and stress reactivity
- Improve emotional regulation and mood stability
- Possibly increase oxytocin in certain practices
- Reduce inflammatory burden
- Buffer your brain’s response to hormonal turbulence
- Support quality of life during your longest life chapter
**That’s not mystical thinking. That’s applied neuroscience—with the humility to admit what we don’t yet know.**
-----
## Three Things to Try This Week
**1. Set a stupidly small goal**
Five minutes. One conscious breath cycle. Build the habit before worrying about technique or tradition.
**2. Choose a practice that resonates culturally**
If silent seated meditation feels alien, try:
- Rhythmic breathwork with music
- Walking meditation in nature
- Heart-focused attention (Heartfulness or loving-kindness)
- Community-based practice
Your nervous system doesn’t care about authenticity to ancient traditions—it cares about what creates safety and presence for *you*.
**3. Track your subjective experience, not enlightenment**
How’s your sleep? Your emotional reactivity? Your capacity to handle what comes? Those are your metrics. Give yourself 30 days of consistent practice—that’s how long it took to produce measurable hormonal changes in controlled studies.
-----
Your brain is listening.
Your hormones are shifting.
The practice that helps you navigate both might be simpler—more culturally diverse, and more evidence-based—than the wellness industry wants you to believe.
-----
**What part of your hormonal journey are you navigating right now? And what contemplative traditions (seated meditation, rhythmic movement, communal practice, breathwork) feel most authentic to your nervous system? Drop a comment—I’m genuinely curious.**
-----
*Research citations and full studies are woven throughout. Because extraordinary claims require more than good vibes—they require receipts, context, and intellectual honesty.*